Diabetes
About Diabetes
What is Diabetes?
Diseases caused by diabetes
1. Diseases due to disorders in small vessels:
Retinopathy: The risk of this disease is that people with diabetes have a 25-fold higher risk of being blind than those without diabetes.
Neuropathy: It develops in about half of diabetics. Burns, numbness, tingling, pinching and pain occur in the feet.
Nephropathy: Nephropathy develops in 5 to 15% of patients with type 2 diabetes, leading to a reduction in renal function.
2. Diseases due to disorders in large vessels:
Coronary Artery Diseases (Obstructions in the Heart-Feeding Veins): It is the main cause of cardiovascular disease, morbidity and mortality in diabetic patients.
Peripheral Vascular Diseases, Cerebrovascular Diseases (Bleeding and Occlusion Related to Cerebral Vessels, Diseases Related to Non-Vessel Causes: Gastroparasis (nausea, vomiting, premature saturation, abdominal distention), diarrhea or constipation, infectious (pneumonia, urinary tract infections, skin and soft tissue infections), dermatological findings (late wound healing and skin ulceration, diabetic skin spots, genitourinary dysfunction).
Methods of Diabetes Treatment
The aim of the treatment of diabetes is to keep blood sugar in the normal range and to prevent micro and macro vascular complication due to diabetes, to increase life time and quality.
Diabetes treatment begins with lifestyle changes, primarily involving patient education, healthy eating and exercise. Despite the change of lifestyle, if the blood sugar does not return to normal oral antidiabetic what we call oral pills and blood sugar is tried to keep within normal limits. When this treatment is not sufficient, insulin treatment can be started.
Patient Education and Healthy Nutrition:
It is one of the main treatment steps in diabetes control. The aim is to provide the desired metabolic control by providing adequate and balanced nutrition habits, to prevent the chronic copulations of diabetes, to improve the quality of life by providing self-management skills in the problems that may be encountered during the day (hypoglycemia, acute disease). With healthy diet therapy, a reduction of 1% can be achieved in patients with type 1 diabetes at HbA1c levels and a reduction of 1-2% can be achieved in patients with type 2 diabetes.
Exercises:
Physical activity is as important as healthy nutrition and medication.
Regular exercise contributes to the prevention of the development of type 2 diabetes by decreasing insulin resistance in people with prediabetes and increasing the use of sugar by muscle tissue. In people with type 2 diabetes, it facilitates regulation of blood sugar levels, lipid levels and blood pressure control. The exercise program differs according to the individual, in order to benefit, it should include programs running all the body muscles at least 3 times a week, walking, swimming for 20-30 minutes and so on.
It has been shown in the diabetes prevention program study carried out in United States that incidence of diabetes decreases by 58% in terms of lifestyle changes, gaining healthy eating habits, regular exercise and training.
Oral Antidiabetic Drugs:
They are drugs that are taken by mouth in patients with type 2 diabetes, regulate the release of insulin from the pancreas, and regulate the effect on the target cells or slow the absorption of glucose from the intestine.
Sulfonylureas: They induce insulin secretion by stimulating insulin-secreting beta cells from the pancreas. The most significant side effects of sulfonylureas are hypoglycemia and weight gain. It can be taken half an hour before meals or while having meal.
Biguanides: They do not affect the release of insulin from the pancreas. They increase glucose uptake to cells, reducing glucose production in the liver and glucose absorption from the intestines.
Alpha-Glucosidase Inhibitors: Inhibition of alpha-glucosidase enzyme is effective in lowering blood sugar by slowing the breakdown of carbohydrates in the intestine and by preventing glucose absorption.
Inhibin Mimetic Drugs: They act by mimicking the incretins secreted from the intestines or by preventing the incretins from breaking up. Glucagon-like peptide-1 (GLP-1) analogs (exenatide, liraglutide, etc.) are used by injection. GLP-1 analogs do not increase the risk of hypoglycemia and also have weight-loss-promoting effects.
DPP-4 Inhibitors: They act by inhibiting the dipeptidyl peptidase-4 (DPP-4) enzyme and by increasing the effect of endogenetretin.
Insulin: In individuals without diabetes, after each meal, the pancreas produces insulin to transform the nutrients taken into energy. In diabetics, the pancreas cannot produce enough insulin, or the insulin produced cannot be used in target cells (muscle, fat and liver cells). In this case, we need to provide insulin that is vital for our body. There are several types of insulin used today. They are grouped as human insulin and analog insulin, as well as short, medium and long-acting.
Metabolic Surgery: The treatment of diabetes by surgery. These surgeries not only control blood sugar, but also greatly improve problems such as hypertension, dyslipidemia (high triglyceride, low HDL), sleep apnea, burns in hands and feet related to neuropathy, retinopathy and fatty liver.
Diabetes Surgeries
Ileal Interposition
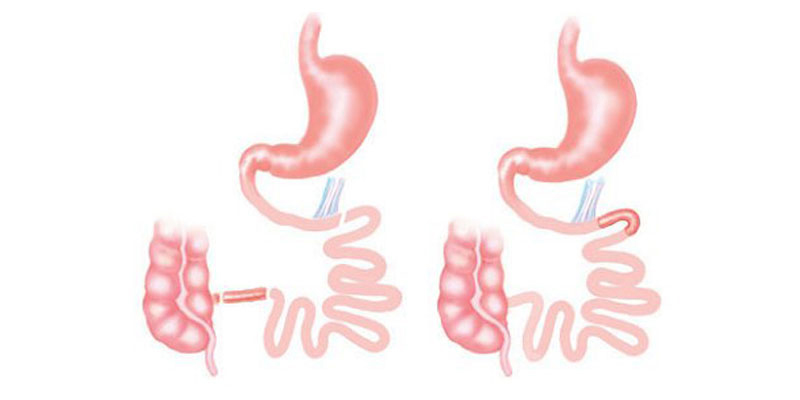
It is a metabolic (diabetes) surgery. The feature that distinguishes this operation from the others is basically the process of displacement in the small intestine. Food passage from all small intestine is available. First of all, sleeve gastrectomy (stomach reduction) procedure is applied to dislodge the left outer part of the stomach in relation to the patient's BMI. Then, a part between 150-200 cm of the small intestine is taken from its last part and carried to the front part of the stomach. The food, thus, taken enters the last part of the small intestine after the stomach.
Type 2 diabetes (diabetes mellitus), blood pressure, cholesterol and metabolically associated diseases are controlled after this procedure.
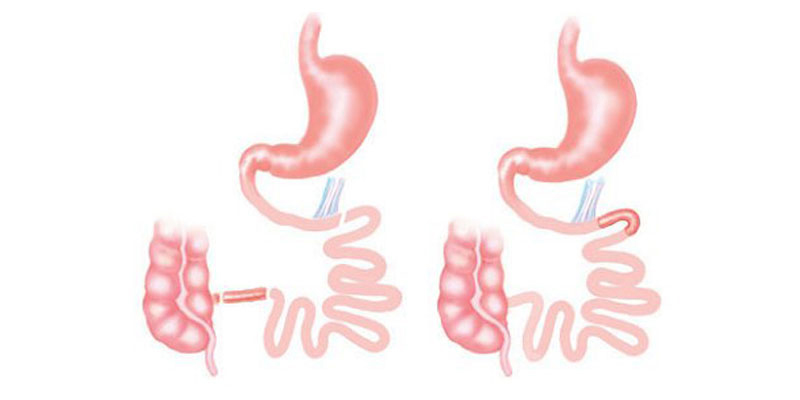
Transit Bipartition
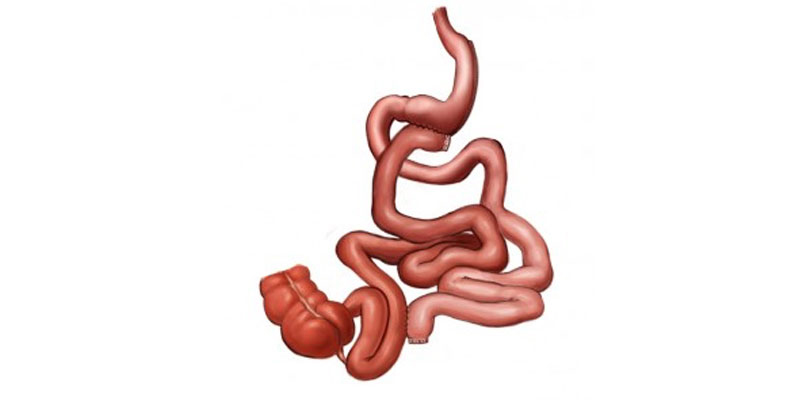
Nowadays, it is a widely applied technique. In addition to patients with Type 2 diabetes (diabetes mellitus), this surgery technique can be performed in obese individuals with Transit Beeping operation.
The difference from all other operations is can be preferred even for individuals with osteoporosis and iron deficiency due to short duration, absorptive procedure and activation of duodenum.
In addition to the operation of the sleeve gastrectomy (stomach reduction) with this operation, 80-120 cm trietze (beginning of the small intestine) is calculated starting from the last part of the intestine and this point is marked. From the marked area, 150 cm is calculated more and the small intestine is cut from 230-270 cm. The lower end of the small intestine which has been cut is attached to the stomach. The upper end of the small intestine is attached to the previously marked 80-120 cm. Thus, 1/3 of the foods we eat naturally pass through duodenum. 2/3 of them pass throughthe new connection to the stomach.
Type 2 diabetes (diabetes mellitus), blood pressure, cholesterol and metabolically associated diseases are controlled after this procedure.
What is Diabetes?
- In diabetes, symptoms such as drinking too much water, frequent urination and eating too much are seen and the patient's blood sugar level is over 200 mg/dl at any time.
- Fasting blood sugar is detected twice over 126 mg/dl.
- In the second hour of oral glucose tolerance test, blood sugar level is above 200 mg/dl.
- The HbA1c value is determined over 6.5%.
Diseases caused by diabetes
1. Diseases due to disorders in small vessels:
Retinopathy: The risk of this disease is that people with diabetes have a 25-fold higher risk of being blind than those without diabetes.
Neuropathy: It develops in about half of diabetics. Burns, numbness, tingling, pinching and pain occur in the feet.
Nephropathy: Nephropathy develops in 5 to 15% of patients with type 2 diabetes, leading to a reduction in renal function.
2. Diseases due to disorders in large vessels:
Coronary Artery Diseases (Obstructions in the Heart-Feeding Veins): It is the main cause of cardiovascular disease, morbidity and mortality in diabetic patients.
Peripheral Vascular Diseases, Cerebrovascular Diseases (Bleeding and Occlusion Related to Cerebral Vessels, Diseases Related to Non-Vessel Causes: Gastroparasis (nausea, vomiting, premature saturation, abdominal distention), diarrhea or constipation, infectious (pneumonia, urinary tract infections, skin and soft tissue infections), dermatological findings (late wound healing and skin ulceration, diabetic skin spots, genitourinary dysfunction).
Methods of Diabetes Treatment
The aim of the treatment of diabetes is to keep blood sugar in the normal range and to prevent micro and macro vascular complication due to diabetes, to increase life time and quality.
Diabetes treatment begins with lifestyle changes, primarily involving patient education, healthy eating and exercise. Despite the change of lifestyle, if the blood sugar does not return to normal oral antidiabetic what we call oral pills and blood sugar is tried to keep within normal limits. When this treatment is not sufficient, insulin treatment can be started.
Patient Education and Healthy Nutrition:
It is one of the main treatment steps in diabetes control. The aim is to provide the desired metabolic control by providing adequate and balanced nutrition habits, to prevent the chronic copulations of diabetes, to improve the quality of life by providing self-management skills in the problems that may be encountered during the day (hypoglycemia, acute disease). With healthy diet therapy, a reduction of 1% can be achieved in patients with type 1 diabetes at HbA1c levels and a reduction of 1-2% can be achieved in patients with type 2 diabetes.
Exercises:
Physical activity is as important as healthy nutrition and medication.
Regular exercise contributes to the prevention of the development of type 2 diabetes by decreasing insulin resistance in people with prediabetes and increasing the use of sugar by muscle tissue. In people with type 2 diabetes, it facilitates regulation of blood sugar levels, lipid levels and blood pressure control. The exercise program differs according to the individual, in order to benefit, it should include programs running all the body muscles at least 3 times a week, walking, swimming for 20-30 minutes and so on.
It has been shown in the diabetes prevention program study carried out in United States that incidence of diabetes decreases by 58% in terms of lifestyle changes, gaining healthy eating habits, regular exercise and training.
Oral Antidiabetic Drugs:
They are drugs that are taken by mouth in patients with type 2 diabetes, regulate the release of insulin from the pancreas, and regulate the effect on the target cells or slow the absorption of glucose from the intestine.
Sulfonylureas: They induce insulin secretion by stimulating insulin-secreting beta cells from the pancreas. The most significant side effects of sulfonylureas are hypoglycemia and weight gain. It can be taken half an hour before meals or while having meal.
Biguanides: They do not affect the release of insulin from the pancreas. They increase glucose uptake to cells, reducing glucose production in the liver and glucose absorption from the intestines.
Alpha-Glucosidase Inhibitors: Inhibition of alpha-glucosidase enzyme is effective in lowering blood sugar by slowing the breakdown of carbohydrates in the intestine and by preventing glucose absorption.
Inhibin Mimetic Drugs: They act by mimicking the incretins secreted from the intestines or by preventing the incretins from breaking up. Glucagon-like peptide-1 (GLP-1) analogs (exenatide, liraglutide, etc.) are used by injection. GLP-1 analogs do not increase the risk of hypoglycemia and also have weight-loss-promoting effects.
DPP-4 Inhibitors: They act by inhibiting the dipeptidyl peptidase-4 (DPP-4) enzyme and by increasing the effect of endogenetretin.
Insulin: In individuals without diabetes, after each meal, the pancreas produces insulin to transform the nutrients taken into energy. In diabetics, the pancreas cannot produce enough insulin, or the insulin produced cannot be used in target cells (muscle, fat and liver cells). In this case, we need to provide insulin that is vital for our body. There are several types of insulin used today. They are grouped as human insulin and analog insulin, as well as short, medium and long-acting.
Metabolic Surgery: The treatment of diabetes by surgery. These surgeries not only control blood sugar, but also greatly improve problems such as hypertension, dyslipidemia (high triglyceride, low HDL), sleep apnea, burns in hands and feet related to neuropathy, retinopathy and fatty liver.
Diabetes Surgeries
- Ileal interposition
- Transit bipartition
Ileal Interposition
It is a metabolic (diabetes) surgery. The feature that distinguishes this operation from the others is basically the process of displacement in the small intestine. Food passage from all small intestine is available. First of all, sleeve gastrectomy (stomach reduction) procedure is applied to dislodge the left outer part of the stomach in relation to the patient's BMI. Then, a part between 150-200 cm of the small intestine is taken from its last part and carried to the front part of the stomach. The food, thus, taken enters the last part of the small intestine after the stomach.
Type 2 diabetes (diabetes mellitus), blood pressure, cholesterol and metabolically associated diseases are controlled after this procedure.
Transit Bipartition
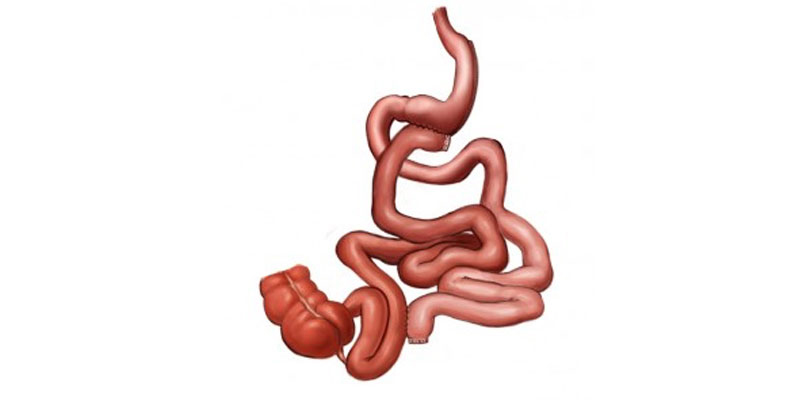
Nowadays, it is a widely applied technique. In addition to patients with Type 2 diabetes (diabetes mellitus), this surgery technique can be performed in obese individuals with Transit Beeping operation.
The difference from all other operations is can be preferred even for individuals with osteoporosis and iron deficiency due to short duration, absorptive procedure and activation of duodenum.
In addition to the operation of the sleeve gastrectomy (stomach reduction) with this operation, 80-120 cm trietze (beginning of the small intestine) is calculated starting from the last part of the intestine and this point is marked. From the marked area, 150 cm is calculated more and the small intestine is cut from 230-270 cm. The lower end of the small intestine which has been cut is attached to the stomach. The upper end of the small intestine is attached to the previously marked 80-120 cm. Thus, 1/3 of the foods we eat naturally pass through duodenum. 2/3 of them pass throughthe new connection to the stomach.
Type 2 diabetes (diabetes mellitus), blood pressure, cholesterol and metabolically associated diseases are controlled after this procedure.
Share